About Dr. Mona Naman Shah
MMBS, MD, Robotic Surgeon , OBGY fellowship in Gynecologic Oncology from Christian Medical College, Vellore with extensive trainings of open and laparoscopic surgical techniques
Robotic Gynecology
Advanced precision in gynecologic care.
Gynecology Cancer
Specialized care for gynecologic cancers.


Our Best Services
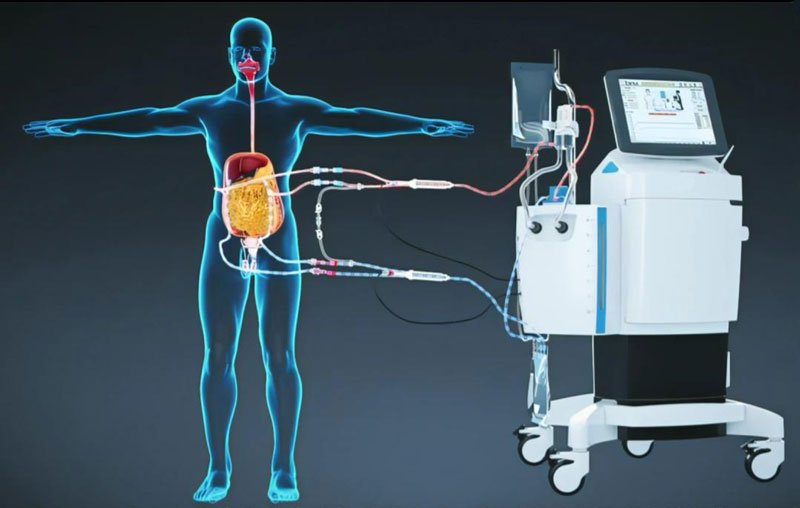
HIPEC
Dr. Mona Naman Shah is a renowned gynecologist and gynec oncosurgeon in Ahmedabad, specializing in laparoscopic and robotic surgeries, comprehensive gynecologic cancer care and advanced HIPEC treatment.
Uterus Cancer Clinic
Uterus Cancer Clinic offers expert diagnosis, advanced surgical and non-surgical treatments, and personalized care for women with uterine cancers, ensuring better outcomes with best compassion and precision.
Ovarian Cancer Clinic
Ovarian Cancer Clinic provides specialized diagnosis, best advanced treatment options, and personalized care for women with ovarian cancer, focusing on early detection, precision surgery, and improved outcomes.

Female Cancer Clinic
Female Cancer Clinic provides expert diagnosis, advanced treatment, and compassionate care for all types of women’s cancers, ensuring holistic support from detection to recovery.

Cervix Cancer Clinic
Cervix Cancer Clinic offers specialized diagnosis, advanced treatment, and compassionate care for cervical cancer, focusing on early detection and improved recovery outcomes.
Immediately Call Gynaecology Care
Phone Number: +91 98795 05063
0
k+
0
+
0
+
0
+
Where Expertise Meets Compassion
Advanced Robotic Surgery
Swift recovery through advanced surgical precision.
Gynecologic Cancer Care
Comprehensive care for all types of gynecologic cancers.
Patient Support
Dedicated care, every step of the way.

What Our Happy Patient Says
Common Questions, Clear Answers